Each year, around 3,500 babies die of a sleep-related cause. While the number is staggering, safe sleep practices can help keep your baby safe and limit the risk.
 There are a couple different terms used to describe when a baby dies of an unknown cause. The overarching term is SUID, which stands for “sudden unexplained infant death.” When this occurs during sleep, the more specific term is SIDS, which stands for “Sudden Infant Death Syndrome.”
There are a couple different terms used to describe when a baby dies of an unknown cause. The overarching term is SUID, which stands for “sudden unexplained infant death.” When this occurs during sleep, the more specific term is SIDS, which stands for “Sudden Infant Death Syndrome.”
This post is brought to you by our partners at Children’s Hospital at Erlanger.
SIDS is the unexpected death of a child younger than 1 year that remains unexplained even after an autopsy. Most SIDS deaths happen in babies between 1 month and 4 months of age, and the majority (90%) of SIDS deaths happen before a baby reaches 6 months of age. However, SIDS deaths can happen anytime during a baby’s first year. SIDS affects slightly more male children than female. African Americans and Native Americans are at a higher risk than Caucasians.
But while we know these facts, we don’t know exactly what causes SIDS. However, researchers have uncovered some common factors known to contribute to SIDS.
Let’s take a look at those risk factors and how you can protect your little one.
Common factors for SIDS
Certain things place an infant at an increased risk of SIDS. Those factors include:
- The use of soft bedding or unsafe beds, like couches or daybeds
- Overheating due to excessive clothing, blankets or room temperature
- Having a mother younger than age 20
- Having a mother who smoked during pregnancy
- Having a mother who received little or no prenatal care
- Premature birth or low birth weight
- Exposure to secondhand smoke
- Sleeping on the stomach
- The use of loose bedding materials like blankets and pillows
While researchers still aren’t quite certain about many aspects of SIDS, they have identified that it occurs when an infant’s body can’t regulate breathing, heart function, and/or body temperature.
Lowering the risk of SIDS
While there’s no way to entirely mitigate the risk of SIDS, there are safe sleep habits that can lower the risk and protect your baby. First and foremost, always put your baby to sleep on his or her back.
This is an absolute — it’s a proven tactic known to reduce the risk of SIDS. Since the 1990s when the American Academy of Pediatrics and the National Institutes of Health began recommending infants sleep on their backs, the number of SIDS fatalities has dropped by 50 percent.
Both side sleeping and sleeping on the stomach are considered unsafe.
Contrary to some misconceptions, sleeping on the back is not associated with an increased risk of choking or any type of head deformity. The ABC’s of Infant Safe Sleep offers simple guidelines to help you decrease the risk of SIDS.
The ABCs of Infant Safe Sleeping
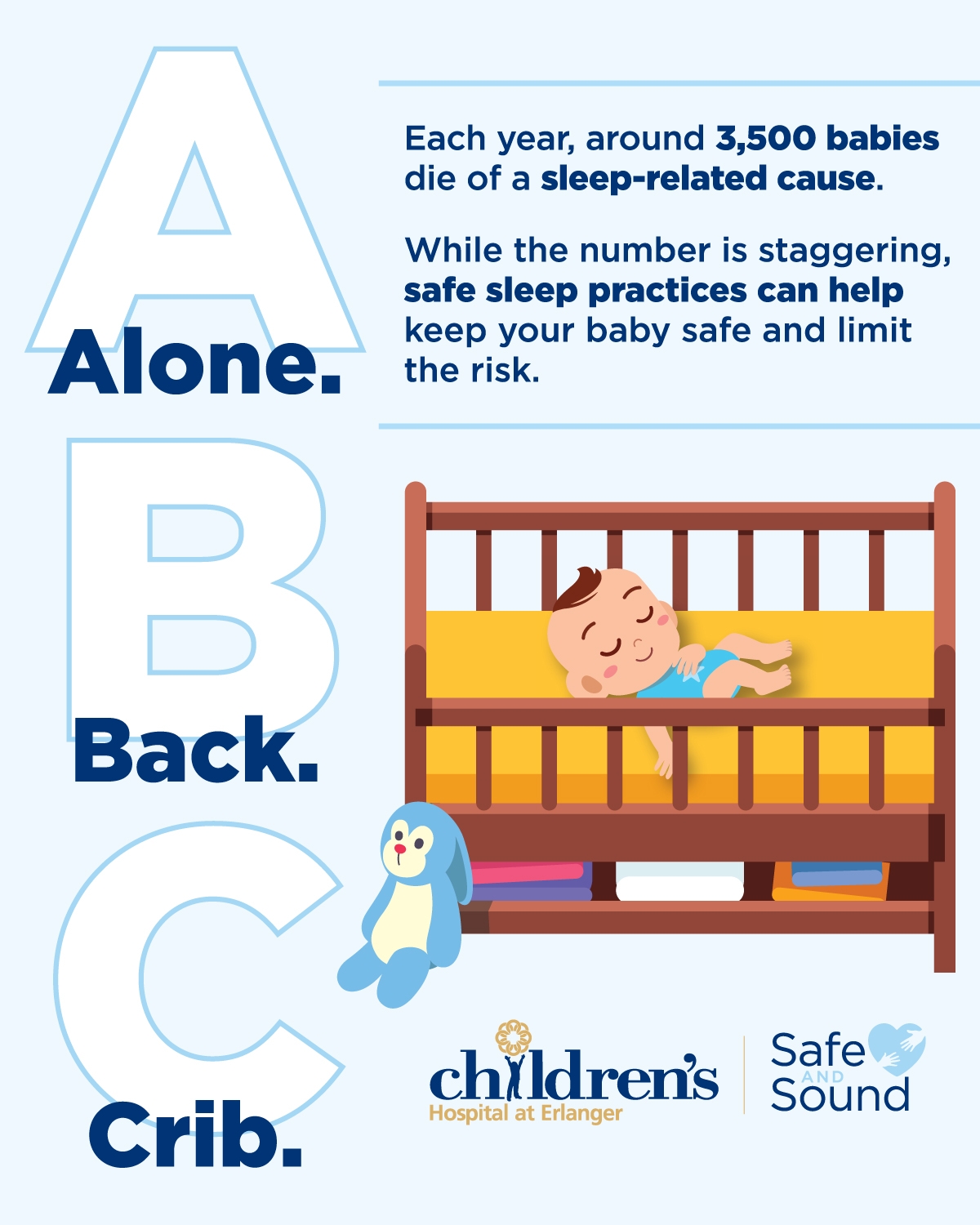 A for Alone
A for Alone
- Put baby to sleep alone in their own crib or bassinet.
- Don’t put baby to bed with other children or adults. They can accidentally suffocate a baby by lying too close to the baby’s mouth or nose, or rolling onto them while asleep.
- Keep all soft items away from baby when sleeping in crib or bassinet. Babies should not sleep with stuffed animals, pillows or blankets – soft items could accidentally fall over a baby’s face and suffocate them.
- A blanket sleeper or sleep sack will keep a baby comfortable. Don’t use heavy blankets or quilts that may overheat the baby.
B for Back
- Put babies to sleep on their backs. Babies who sleep on their backs are much less likely to die of infant sleep-related deaths.
- Teach other mothers, grandmothers and those who care for your baby that “back to sleep” is safest for babies.
- “Back to sleep” will not increase a baby’s risk of choking according to doctors.
C for Crib
- Cribs and bassinets are the safest places for babies to sleep.
- Cribs should be free of pillows, bumpers, stuffed toys, blankets or anything that could
accidentally cover your baby’s face and suffocate them. - Unlike firm crib mattresses, adult beds are soft and can cause babies to suffocate.
- Always return your baby to their crib after nursing. To make breastfeeding easier, keep a crib or bassinet next to your bed.
- Mothers who exclusively breastfeed their baby should discuss infant safe sleeping with their lactation consultant.
Beyond following the “ABC’s of Safe Sleep” guidelines, parents can also follow some other basic measures to help protect their little ones:
Ensure your child has a firm sleeping surface. This has some basic principles — a child should be put to sleep on a mattress in an approved crib covered by a fitted sheet with no other bedding or objects in the crib. Portable cribs or play yards that adhere to the standards of the Consumer Product Safety Commission are also OK.
Ensure your child isn’t sleeping on a bed or couch. Both carry an increased risk of suffocation, putting your little one at risk.
Ensure no hazards are within grabbing distance. Take a careful look around the crib to make sure there are no window blind cords, electrical wires or other potential strangulation hazards nearby. Even if your baby doesn’t move around much, this is still important to consider.
Ensure your child’s head and face remain uncovered. The AAP doesn’t recommend putting your baby to sleep with any items in the crib. But if you do use a blanket, make sure it stays away from the baby’s mouth. The blanket should go up no higher than the baby’s chest.
Keep your little one at a comfortable temperature. Your baby doesn’t need to be warmer than you do. Set the temperature at a level that feels comfortable to you — and don’t add excessive layers to your child’s clothing.
Consider giving your child a pacifier. This one might seem a bit out of the ordinary, but studies have shown that pacifiers may reduce the risk of SIDS. Give your child a pacifier when laying him or her down to sleep, but there’s no need to reinsert it if it comes out, unless your little one needs it.
Avoid exposing your baby to smoke. Secondhand smoke is a risk factor for SIDS. So make sure that no one who’s around your little one smokes.


















